multi epitop vaccination versus breast cancer micrometastasis
- Martin Döhring

- 26. Sept. 2025
- 4 Min. Lesezeit
### Addressing Early Micrometastasis in Breast Cancer with mRNA Vaccination Strategy ...early-onset micrometastasis represents a critical barrier in breast cancer management. These subclinical tumor cell deposits, often disseminating during primary tumor development, evade detection and contribute to ~90% of cancer-related deaths through distant recurrence, even after seemingly successful local therapies like surgery or radiation. Developing an mRNA-based vaccinating strategy targeting common epitopes could provide a proactive, adjuvant approach to elicit systemic antitumor immunity, priming the immune system to surveil and eliminate these disseminated cells before they form overt metastases. Below, I outline a evidence-based framework for such a strategy, drawing from recent preclinical and clinical advances (up to 2025).
#### Core Principles of the Proposed mRNA Vaccine Strategy
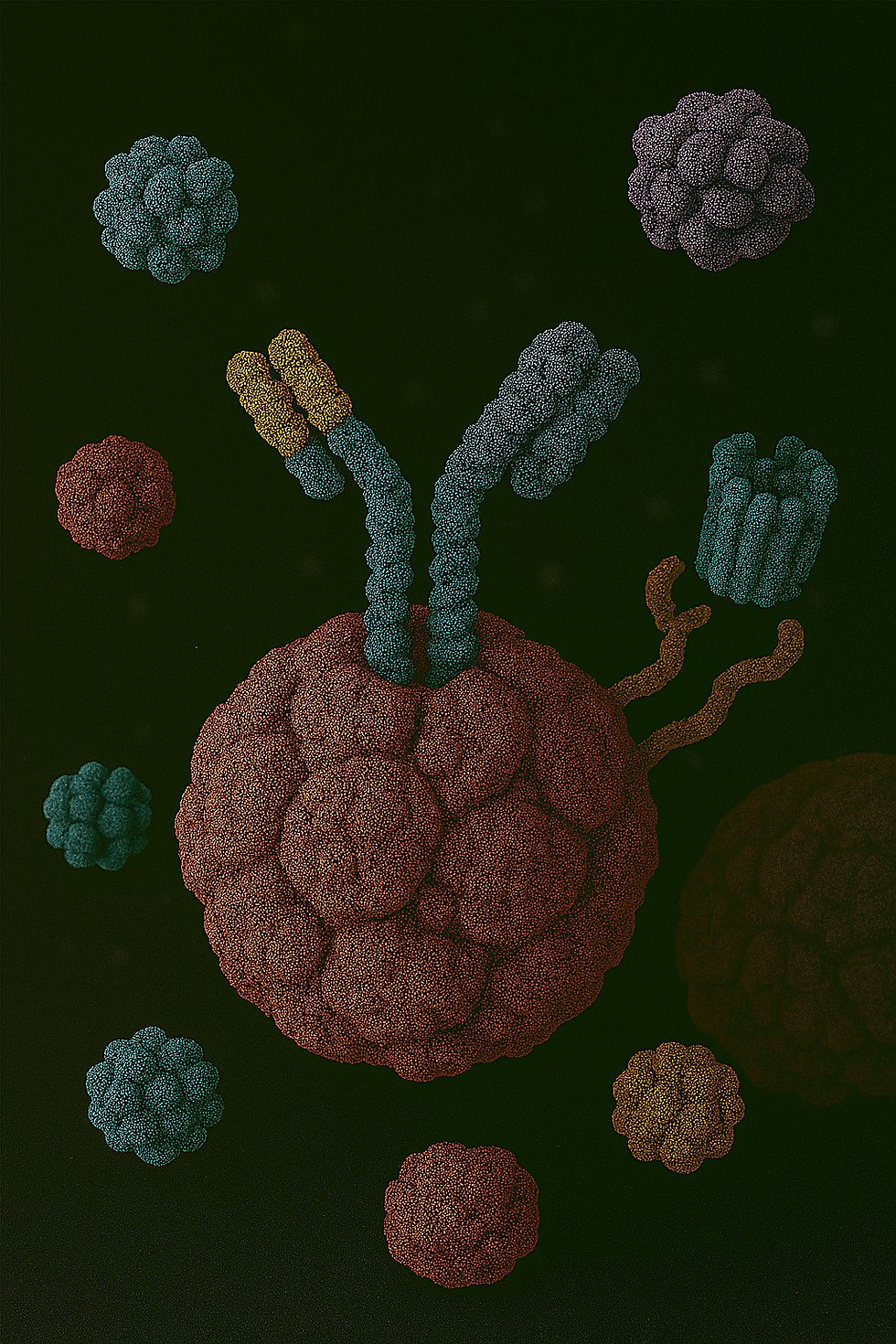
mRNA vaccines are ideal for this context due to their rapid production, ability to encode multiple epitopes, and capacity to induce both humoral (antibody) and cellular (T-cell) responses without genomic integration risks. The strategy focuses on multi-epitope constructs to cover breast cancer heterogeneity (e.g., HER2+, luminal, TNBC subtypes) and promote epitope spreading—where initial immune activation reveals additional tumor antigens, amplifying responses against micrometastatic lesions.
- Target Selection: Common Epitopes
Prioritize tumor-associated antigens (TAAs) overexpressed in >50-80% of breast tumors, with minimal expression in healthy tissues to minimize autoimmunity. Key candidates include:
- HER2 (ErbB2): A transmembrane receptor overexpressed in 15-30% of cases (especially HER2+ subtype); epitopes like p369-379 (HLA-A2-restricted) drive CD8+ T-cell responses.
- MUC1: A mucin glycoprotein aberrantly glycosylated in >90% of breast cancers (ubiquitous across subtypes, including TNBC); targets like STn-MUC1 epitopes elicit antibodies and CTLs.
- MAGE-A family (e.g., MAGE-A3/A6): Cancer-testis antigens in 40-60% of aggressive tumors, linked to metastasis; 9-mer MHC-I epitopes (e.g., MAGE-A3: EVDPIGHLY) for cytotoxic responses.
- Additional shared epitopes: Gal-3 (β-galactoside-binding lectin, overexpressed in 70% of tumors, promotes invasion); MAM-A (membrane-associated mucin, in >80% of cases, correlates with poor prognosis).
These are "common" as they appear across subtypes, enabling a semi-universal vaccine rather than fully personalized neoantigens (though hybrids are feasible).
- Vaccine Design and Delivery
- mRNA Construct: Encode a fusion protein of 4-6 epitopes (e.g., HER2 + MUC1 + MAGE-A + Gal-3) linked by flexible GSST linkers and cleavable disulfides for efficient MHC processing. Include an adjuvant like IL-12 (for Th1 bias) or 4-1BBL (for T-cell costimulation) to enhance dendritic cell (DC) activation. Use codon-optimized, nucleoside-modified mRNA (e.g., pseudouridine) for stability and reduced immunogenicity. Total length: ~600-800 nt for multi-epitope coverage.
- Delivery Platform: Lipid nanoparticles (LNPs) for intramuscular or intranodal injection, targeting lymph nodes for DC uptake. Emerging circRNA-LNPs improve half-life (>48 hours) and potency. Dose: 30-100 μg per epitope, administered in 3-4 priming/boost doses.
- Timing for Micrometastasis Prevention: Adjuvant setting post-surgery (e.g., weeks 4-12), when minimal residual disease persists, to establish long-lived memory T cells (CD8+ central memory) that patrol distant sites like bone, lung, or brain.
#### Mechanism of Action Against Micrometastasis
1. Antigen Presentation and Priming: mRNA transfects DCs, leading to epitope cross-presentation on MHC-I/II, activating naive CD4+ helper and CD8+ cytotoxic T cells.
2. Systemic Surveillance: Induced CTLs infiltrate micrometastatic niches, lysing dormant/disseminated tumor cells via perforin/granzyme. Antibodies (e.g., anti-MUC1 IgG) block invasion/adhesion molecules like Gal-3.
3. Immune Memory and Epitope Spreading: Long-term B/T-cell memory (lasting >1 year) prevents outgrowth; initial responses "unmask" neoantigens in the tumor microenvironment (TME), broadening immunity. This counters TME immunosuppression (e.g., via PD-L1 upregulation).
4. Synergy with Standard Care: Combine with checkpoint inhibitors (e.g., pembrolizumab) or endocrine therapy to boost efficacy, as seen in models where mRNA vaccines + anti-PD-1 reduced recurrence by 50-70%.
Preclinical data support this: In TNBC mouse models, MUC1/HER2 mRNA-LNPs eradicated occult lung micrometastases, extending survival by 40%; multi-epitope designs (MAGE-A + Gal-3) showed 90% population coverage and stable TLR binding for robust IFN-γ production.
#### Current Progress and Clinical Translation
- Preclinical Milestones (2023-2025): Bioinformatics-optimized multi-epitope mRNA vaccines (e.g., MAGE-A/MAM-A/Gal-3) predict high antigenicity (0.7 score) and non-toxicity, with simulations confirming T-cell activation and metastasis inhibition via reduced TGF-β. HER2-directed vaccines cleared DCIS lesions in vivo, preventing progression to invasive disease.
- Clinical Trials:
| Trial ID | Phase | Design | Status (as of 2025) | Key Outcomes |
|----------|-------|--------|---------------------|--------------|
| NCT03632941 | II | HER2 mRNA (AVX901) + pembrolizumab | Recruiting | Enhanced T-cell infiltration; 30% response in metastatic HER2+ |
| NCT02316457 | I | LNP-mRNA (neoantigens + TAAs like MUC1) for TNBC | Active | Safe; poly-epitopic responses in 60% of patients |
| NCT03313778 | I | Personalized multi-epitope mRNA + PD-1 inhibitor | Recruiting | Reduced recurrence risk by 49% in early data (analogous to melanoma trials) |
| NCT04503278 | I/II | mRNA-CAR-T targeting CLDN6 (related to metastasis) | Ongoing | 33% objective responses; epitope spreading observed |
Challenges include HLA variability (addressed by multi-epitope breadth) and TME barriers (mitigated by combinations). Future directions: Phase III trials for adjuvant use in high-risk early-stage patients, with biomarkers like circulating tumor DNA to monitor micrometastasis clearance.
This strategy holds transformative potential—imagine vaccinating high-risk patients (e.g., node-positive) to cut recurrence by 30-50%.








... below is a detailed, conceptual biomarker panel and sampling schedule tailored for an early-phase (first-in-human / Phase 1-style) study of an mRNA multi-epitope breast-cancer vaccine intended to prevent/eradicate early micrometastasis. It lists what to measure, why, and when to sample (timepoints tied to a typical prime/boost regimen).
Study assumptions (for context)
Vaccine schedule: Prime (Day 0) and Boost (Day 21) (adjustable).
Trial population: early-stage or adjuvant breast-cancer patients with resected primary disease and high risk of micrometastasis (biomarker-selected).
Sampling windows are chosen to capture: (A) immediate innate responses and safety (hours → days), (B) adaptive T cell priming/expansion (days → weeks), and (C) durability and longer-term PD/efficacy signals (months).
Biomarker groups (short)
Systemic complement & terminal pathway activation — sC5b-9, C3a, C5a, C3/C4, Bb/Ba,…